Has your period gone AWOL? How to tell the difference between PCOS and Hypothalamic Amenorrhoea
/One of the most common things I see in clinical practice is missing periods - whether it’s a 19 year old woman whose period has been MIA for the last few months, or a 34 year old woman trying to conceive but having wildly irregular cycles, missing periods are a sign that something is not quite right. Perhaps more concerning though, is just how tricky it can be to get an accurate diagnosis. PCOS, hypothalamic amenorrhoea, premature ovarian failure, peri-menopause, hyperprolactinaemia and more can all cause erratic, unpredictable or totally absent cycles, and being able to address the issue requires an accurate diagnosis. Two conditions in particular that are commonly confused are polycystic ovarian syndrome (PCOS) and functional hypothalamic amenorrhoea (FHA). In this article today, I’m going to explore these two conditions, discuss why there can be confusion when it comes to their diagnosis, and teach you how to distinguish between the two.
But firstly, what’s the difference between PCOS and hypothalamic amenorrhoea?
PCOS is a condition characterised by menstrual irregularities associated with insulin resistance or hyperandrogenism (raised male sex hormones, such as testosterone). PCOS often presents with symptoms such as weight gain (or difficulty losing weight), hair loss, acne, hair growth on the face and polycystic ovaries on ultrasound. Infrequent or absent periods are another possible sign of PCOS, as the body fails to ovulate regularly.
In contrast, hypothalamic amenorrhoea occurs when the brain stops communicating with the ovaries, resulting in the absence of a regular menstrual cycle. This may occur for various reasons, but the most common causes of FHA are under-eating, over-exercising, stress or a combination of the three. The primary symptom of amenorrhoea is a missing period, but other symptoms might include low libido, depression and anxiety, feeling cold and having low energy levels.
On paper, these two conditions almost sound like opposites - one is associated with weight gain, the other with weight loss. One is associated with blood sugar dysregulation, whilst the other is associated with under-eating (especially of carbohydrates). And yet both can result in a missing period.
So if these two conditions are so different, why are so many women misdiagnosed?
There are a few factors that can lead to misdiagnosis in women with PCOS or FHA. The first is when PCOS is diagnosed via ultrasound alone. As I discussed in this Facebook post, PCOS cannot be diagnosed via ultrasound alone, and it requires blood tests and clinical assessment to determine its presence. This is in part because BOTH PCOS and FHA can present with polycystic ovaries on ultrasound. This is because the ‘cysts’ are actually developing ovarian follicles, and both conditions can be associated with an increased number of these follicles.
Similarly, some women are misdiagnosed with PCOS because they have a high level of anti-Müllerian hormone (AMH). This is a hormone that is produced in the developing ovarian follicles, and as we’ve already seen, both PCOS and FHA can be associated with an increased number of these follicles. The more follicles, the more of this hormone is produced, meaning both conditions can be associated with a high AMH. This is why studies have found FHA repeatedly being misdiagnosed as ‘lean PCOS’.
Another point to mention is that a woman might be diagnosed with PCOS on the basis of having missing periods, and symptoms like acne or hair loss. That said, hair loss can occur in FHA as well (due to under-nutrition or stress), and symptoms such as acne or depression can occur even in women without PCOS or FHA, so their presence alone is not diagnostic.
The last group of patients who are at risk of misdiagnosis are those who present atypically; that is, they don’t fit the typical picture of PCOS or FHA. For example, it might a very slim girl who actually has PCOS, or perhaps a woman who struggles with her weight but has lost her period due to high stress levels. These patients don’t fit the typical picture for PCOS or FHA, which is why it is so important to work with a specialist in women’s health who can help ensure an accurate diagnosis.
So how can you tell the difference between PCOS and FHA?
The best way to tell the difference between PCOS and FHA is to work with a healthcare professional who specialises in women’s health and who has a comprehensive understanding of the two conditions. Diagnosis then involves thorough case taking, blood tests and in some cases, ultrasound.
Some important questions to consider include:
When did your period first go missing? Was it after a period of stress or weight loss, or perhaps after you started to gain weight?
Have you adopted a low carbohydrate diet or intense exercise regime? Do you have perfectionist tendencies?
What are your other symptoms? Hair growth on the chin, hair loss, acne, weight gain/loss, low libido, depression, anxiety and so on?
Do you have a family history of PCOS?
Have you recently come off the oral contraceptive pill?
Do you have other disorders that might contribute to or cause missing periods, such as a thyroid disorder, pituitary issue or eating disorder?
After discussing these points with your healthcare provider, the next step in diagnosis is getting some comprehensive blood tests, to determine what is happening hormonally. Depending on your presentation, your healthcare provider will advise which are the most appropriate tests to complete, some of which might include:
LH and FSH
Oestradiol
Progesterone
Androgens (testosterone, DHEAS, androstenedione, SHBG and FAI)
Fasting insulin and fasting blood sugars
Thyroid function tests
Prolactin (to assess for other possible causes of amenorrhoea)
AMH (depending on your age and whether causes such as premature ovarian failure or menopause need to be considered)
Ideally, tests like LH and FSH should be tested on Day 2 or 3 of your cycle, to give your healthcare provider the most accurate picture of what is going on. If your cycle is totally absent however, then they can be tested on any day.
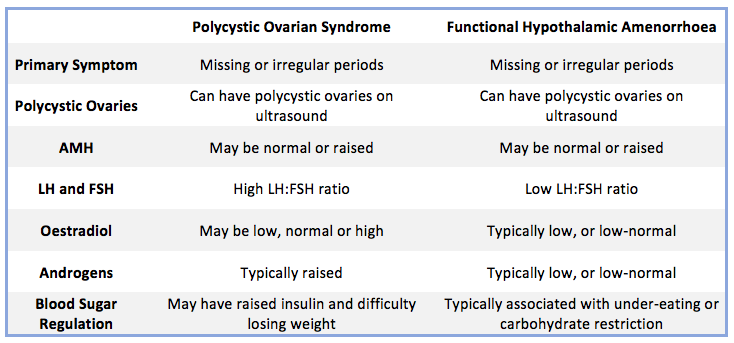
Once these tests have been completed (and other causes of missing periods have been excluded), then your doctor or naturopath can assess the results to determine why your periods have gone AWOL. To summarise some of the key differences, I’ve included a table below that helps differentiate between the typical clinical picture of PCOS and FHA.
Ultimately, if your periods have gone missing, it’s important to work with a qualified healthcare practitioner to determine why. Whilst you might enjoy the simplicity of not having to worry about a visit from Aunt Flow every month, a regular menstrual cycle is a sign of health and fertility. Prolonged amenorrhoea can be associated with undesirable effects such as bone density loss, fertility issues and more, so if your period has gone missing, it’s important to determine why so an appropriate treatment approach can be devised. Stay tuned for future articles on this topic, where I’ll discuss some of the key management approaches for conditions like FHA and PCOS.
Yours in health,
Niki x